What is DES?
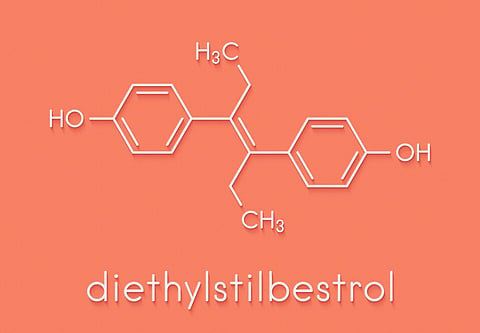
DES is short for diethylstilbestrol, a synthetic estrogen commonly prescribed to help prevent miscarriage and other problems with pregnancy during the years 1938 to 1971. Before the drug was pulled off the market in 1971, an estimated 5 million to 10 million women in the United States and Europe had taken it.
The U.S. Food and Drug Administration recommended its removal in 1971 after studies linked it with a rare form of cancer. Most doctors in this country stopped prescribing the drug at that point, but in parts of Europe DES was still prescribed until the late 1970s and even the early 1980s.
What are the risks associated with this drug?
DES daughters (the term used for women whose mothers took DES during pregnancy) are at greatest risk for health problems, but DES mothers (the women who took the drug) and DES sons may have complications as well.
DES daughters have an increased risk of infertility, ectopic pregnancy, miscarriage, menstrual irregularities, and preterm labor. Twenty-five to 40 percent of DES daughters experience structural abnormalities of the uterus, cervix, or upper vagina. They're more likely, for example, to have a T-shaped or small uterus; they also have a higher chance of developing a cervical hood, a growth on the cervix that usually doesn't require treatment but makes it difficult to use a diaphragm for birth control. DES daughters also have a higher-than-average risk of developing a rare cancer called vaginal clear cell adenocarcinoma. (This risk is still quite low, however -- only one in 1,000.)
DES mothers have an elevated risk of breast cancer, perhaps 30 percent higher than that of other women. DES sons have an increased risk of epididymal cysts, or noncancerous growths, on the backs of the testicles. They may also have an increased risk of other genital abnormalities, including hypospadias (a misplaced opening of the penis), or a smaller than normal penis. However, the evidence of these risks is inconclusive.
One study found that even granddaughters of women who took DES may suffer a small but above-average risk of vaginal clear cell adenocarcinoma. However, a small follow-up study found no such risks. A separate study in the Netherlands found that hypospadias was 20 times more frequent among sons of DES daughters than among the general population.
What is clear cell adenocarcinoma?
It's a rare cervical or vaginal cancer that most commonly affects young women (from age 15 through the early twenties). It can be treated only if caught in the early stages of development. To stop the cancer, women usually must have a radical hysterectomy (removal of the uterus, fallopian tubes, and ovaries) along with a partial or entire removal of the vagina, which requires reconstruction. Clear cell cancer was even more rare before the use of DES; in fact, it was the rise in the number of cases of this cancer that first alerted the medical community to problems associated with DES.
What should I do if I took DES?
If you're a mother who took DES, make sure that your children (no matter how old they are) are regularly examined and tested for problems associated with the drug. Because of your increased risk of breast cancer, you should have annual breast exams and mammograms in addition to checking yourself for lumps every month.
What should I do if my mother took DES?
If you know or suspect that your mother took DES, ask your doctor to give you a DES exam. This screening includes:
- A visual exam of the vagina and cervix for particular abnormalities
- Cervical and vaginal pap smears (the vaginal test checks all four quadrants of the vagina)
- A physical exam (palpation) of the walls of the vagina, uterus, cervix, and ovaries to check for lumps
- Iodine staining of the cervix and vagina to check for abnormal tissues or noncancerous abnormal growths of glandular tissue
You might also want to get a biopsy of your cervix to check for cancer.
DES exams usually cost at least $200 and aren't covered by all insurance plans; also, many doctors haven't been trained to perform this exam. If your regular doctor isn't familiar with it, contact one of the consumer-rights groups for people affected by DES, and ask for a referral to a doctor who is. You can find a list of DES advocacy organizations on the U.S. Centers for Disease Control's DES resource page online (http://www.cdc.gov/DES/consumers/resources/org_advocacy.html).
Besides getting a DES exam, you need to be aware of problems that may occur if you get pregnant. Although most DES daughters can conceive and carry a child to term, they are more susceptible to miscarriage, premature delivery, and tubal pregnancy than are other women. Talk to your physician about these possible complications.
You should also have annual pelvic exams, including a pap smear, because of the higher-than-average risk of clear cell vaginal cancer. Although studies haven't found an increased breast cancer risk for DES daughters, some experts recommend that they be vigilant about doing monthly self-exams and have annual mammograms after they reach the age of 40.
If you're a DES son, you'll be glad to know that most men exposed to DES before birth have no resultant health problems. There is an increased risk of problems with genital organs, however, ranging from harmless irregularities to conditions that may need treatment. Since noncancerous testicular cysts are the most common abnormality, be sure to do monthly exams of your testicles and to promptly report any lumps to your doctor. You don't need to have noncancerous cysts treated unless they're painful.
Where can I learn more about DES?
The U.S. Centers for Disease Control and Prevention maintains its DES web site at http://www.cdc.gov/DES/. Here, readers who aren't sure whether they were exposed to DES can take a self-assessment to help them determine the likelihood of their exposure. Continuing research results will be posted here, as well as general information about DES exposure.
References
Center for Disease Control. DES Update for Consumers, Health Care Providers, and DES Update Partners.
Kaufman RH et al. Continued follow-up of pregnancy outcomes in diethylstilbestrol-exposed offspring. Obstet Gynecol 96(4):483-9.
Titus-Ernstoff L, et al. Long-term cancer risk in women given diethylstilbestrol (DES) during pregnancy. Br J Cancer Jan 5;84(1):126-33.
Brigham Narins, Editor. World of Health: 309-310.
CDC launches new comprehensive information resource about exposure to diethylstilbestrol . CDC Press Release.
Centers for Disease Control. Potential Health Risks for 3rd Generation (Offspring of DES Daughters and Sons).M
Centers for Disease Control. Known Health Effects for DES Sons.